The worldwide spread of COVID-19 has everyone questioning how to protect themselves and help those on the front line of the coronavirus. The CDC recommends facemasks be used for those that have COVID-19 or are showing symptoms and now for anyone in areas with significant community-based transmission. Facemasks are also crucial to healthcare workers and those taking care of someone infected with the virus. Some innovative people are making DIY masks to donate to hospitals in critical need. The next natural question that arises is how well do these homemade masks work? How would their effectiveness be measured? In this two-part series, we will look at the differences between the recommended masks and other materials. In part two, we will examine the different materials that are being recommended for DIY facemasks.
Figure 1 shows an example of particle capture by masks allowing clean air to pass through. Different materials determine how effective masks are, but the two basic features masks need to be effective are:
- Capturing or filtering the virus particles
- Allowing comfortable breathability for longer durations
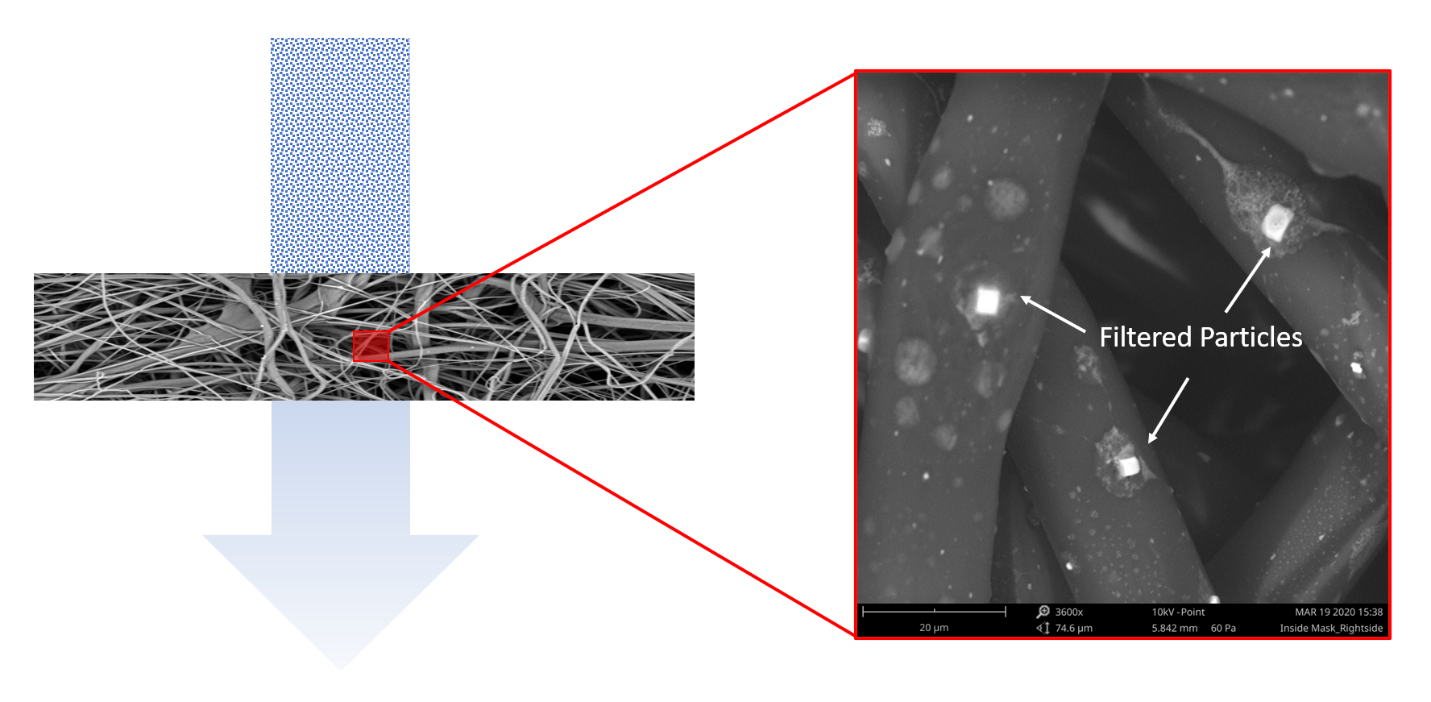
Figure 1. An illustrative example of particle capture by a fiber-based filter
The filtration level of a mask, however, depends on the fiber, the way it’s manufactured, the web’s structure, and the fiber’s cross-sectional shape. Usual surgical masks are three-ply (three layers). This three-ply material is made up from a melt-blown material placed between non-woven fabric. The melt-blown material acts as the filter that stops microbes from entering or exiting the mask. The figure below shows the fiber structure of the outside layer, middle layer and the inner layer. The middle layer is really the key to stopping the virus particles.
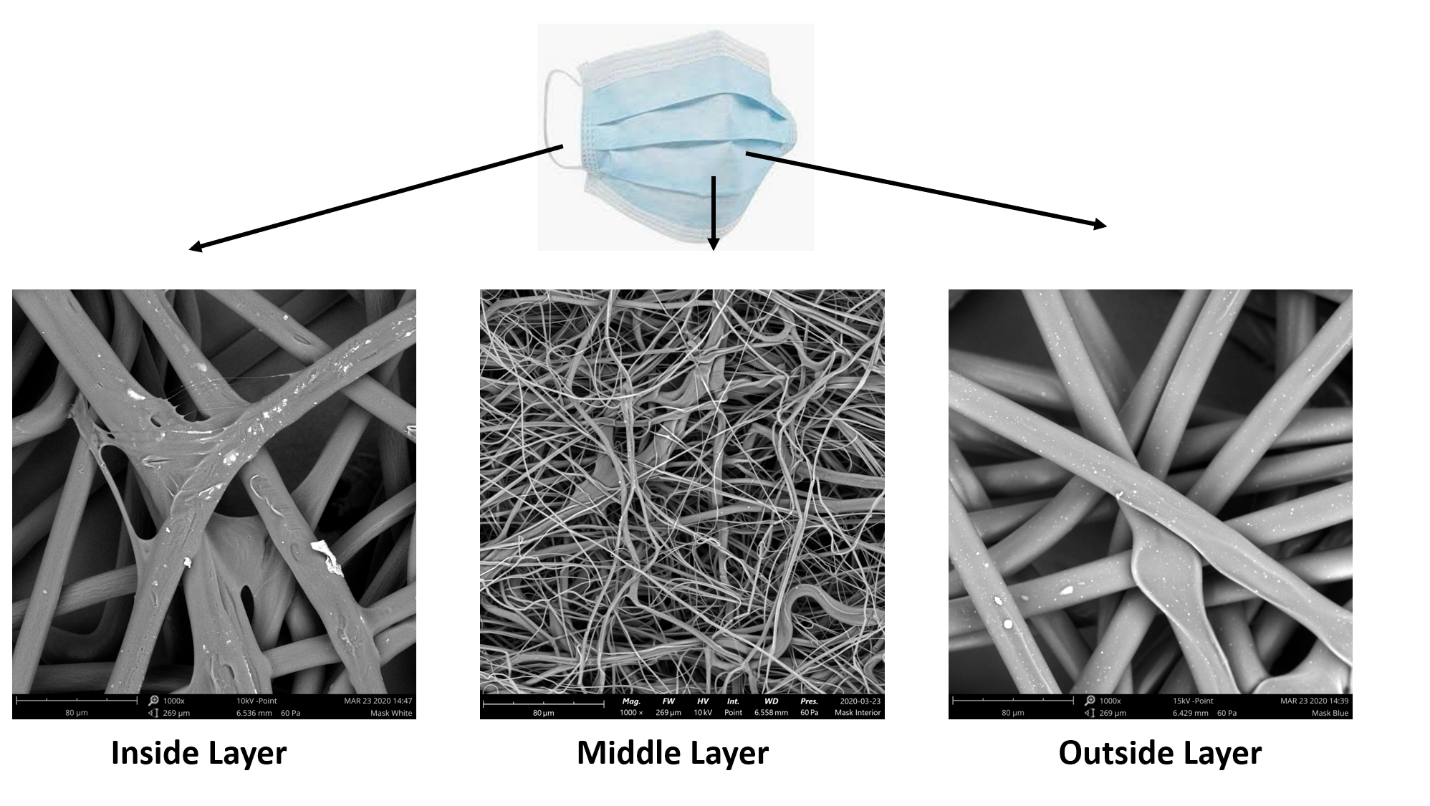
Figure 2. SEM images showing the fiber structure of different layers of surgical mask
These masks prevent large droplets of bodily fluids that may contain viruses or other germs from escaping via the nose and mouth. They also protect against splashes and sprays from other people, such as those from sneezes and coughs. The effectiveness of the mask depends on the fiber structure and porosity. Fiber diameter analysis is one important factor for determining the effectiveness of the masks and needs to be performed on large areas to give us meaningful results. Nanoscience Instruments sells the Phenom desktop SEMs which features an automated fiber analysis package that can be used for companies who are urgently developing their process to backfill the supply chain for the medical community. The automated analysis can be completed in minutes, generating hundreds of images and rich data needed for fast decision-making. Figure 3 shows the automated image analysis performed on a set of fibers showing the mean diameter which translates into the effectiveness of the masks.
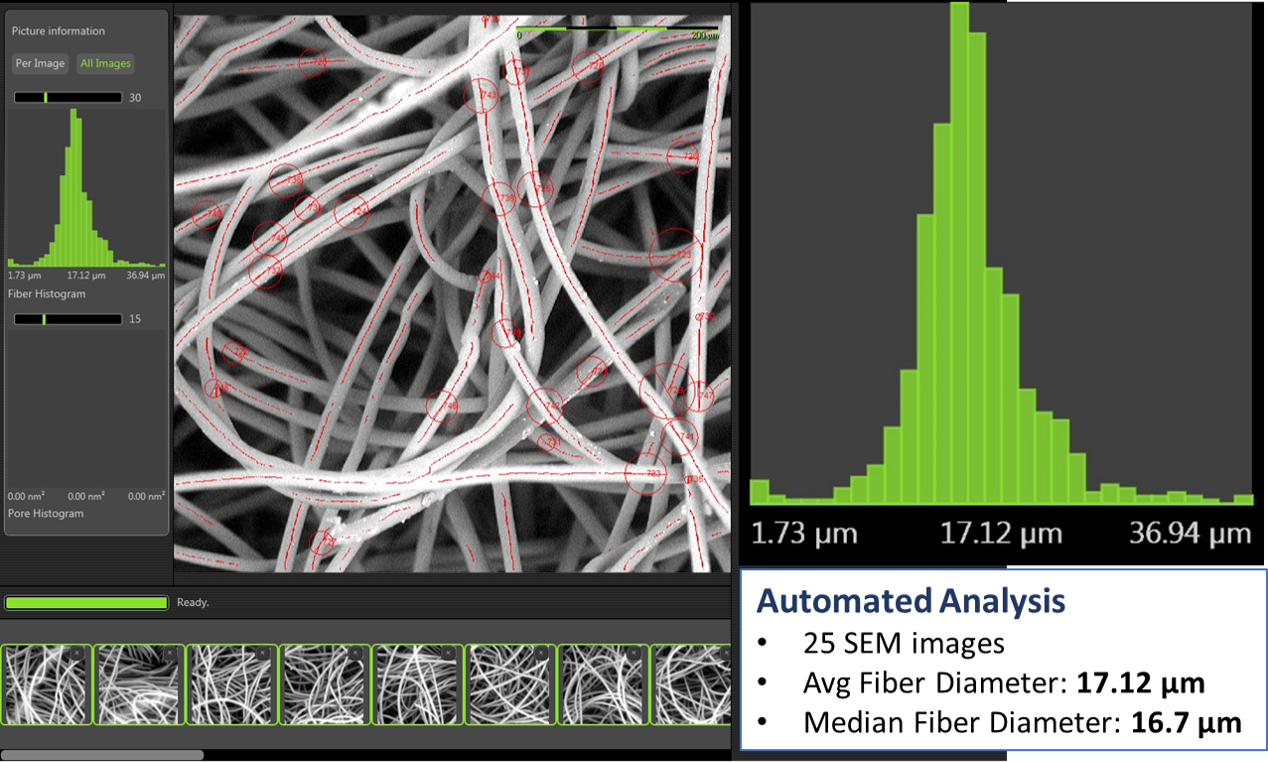
Figure 3. Automated fiber analysis imaged on a Phenom desktop SEM by Thermo Fisher Scientific
The best mask is thus the one having the highest filtering efficiency and lowest airflow resistance, which means mask performs best in blocking airborne particles and provided the best air permeability, enabling the users to breathe freely. Fiber structure is usually a very good indicator of a material’s usability for a mask. Using Thermo Fisher Scientific’s Phenom desktop SEM with automated fiber analysis (FiberMetric), mask manufactures can quickly confirm that their design criteria are met, avoiding delays in the production process. Nanoscience Analytical can also help answer your questions related to fiber analysis with 24 hours turnaround time.
There are several articles floating on the internet with recommended materials for DIY masks with the best options being cotton t-shirts and pillowcases. In part two of our analysis of materials, we will use the Phenom desktop SEM to evaluate the different recommended materials.
References:
- Liu, Zhiqing et al., “Understanding the factors involved in determining the bioburdens of surgical masks.” Annals of translational medicine vol. 7,23 (2019): 754
- Davies, Anna, et al. “Testing the Efficacy of Homemade Masks: Would They Protect in an Influenza Pandemic?” Disaster Medicine and Public Health Preparedness, vol. 7, no. 4, 2013, pp. 413–418
- https://www.deccanherald.com/international/hiv-drugs-touted-as-weapon-in-war-on-coronavirus-801386.html
